Understanding Insomnia: Everything You Need to Know
You can’t imagine anything more frustrating. Every day you’re more exhausted, yet every night, you struggle to fall asleep.
You’ve finally had enough of glancing at the alarm clock or staring blankly at the ceiling for hours. It’s time to do something about the endless tossing and turning rough mornings, and hoping that caffeine will carry you through the day.
You’re here to find out the types, causes, risk factors, symptoms, diagnosis, treatment, complications, and prevention of insomnia. And we’re here to provide the answers.
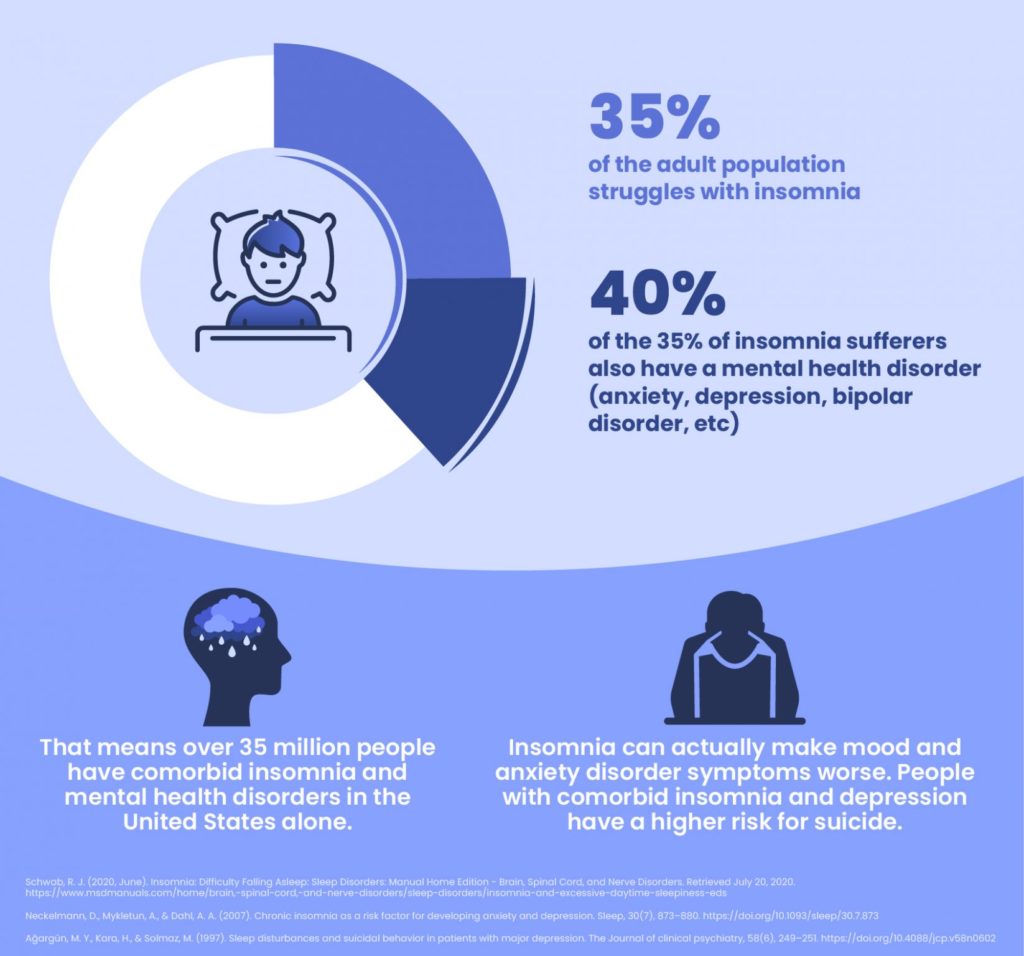
You should know you’re not alone., As many as 33% to 55% of adults experience insomnia symptoms. Keep reading for all the information to help you fall asleep faster, stay asleep longer, and wake up and live better.
What Is Insomnia?
The American Academy of Sleep Medicine defines insomnia as difficulty falling or staying asleep. In addition, some people with insomnia also wake up too early.
Since the average person needs seven to nine hours of sleep to function optimally, frequently struggling to sleep can quickly begin to encroach on daytime activities and energy
It’s normal to miss out on sleep once in a while due to predictable causes like stress or disruptions in your routine. However, if you experience ongoing issues with sleep, and it is negatively impacting your life, including work and personal relationships, you owe it to yourself to investigate further and find a solution.

What are the Types of Insomnia?
First, ask yourself, how long/how often do I have insomnia? How would I characterize my insomnia?
Insomnia can manifest in a variety of ways. Over time or depending on the circumstances, different people may experience one or more of the following types:
Chronic Insomnia
Doctors characterize chronic insomnia as sleep difficulties persisting at least three times per week over at least three months.
Chronic, ongoing insomnia ails about 10% of people, causing severe symptoms interfering with their professional/academic performance and personal life.
Acute Insomnia
Affecting roughly 15% to 20% of adults, acute, or short-term insomnia often follows life stressors like illness and loss or grief. Acute insomnia can also be more prevalent in light sleepers.
Some people with acute insomnia may find it develops into chronic insomnia. But fortunately, 75% of Americans who notice short-term sleep problems won’t develop long-term insomnia.
Other Types:
Sleep-onset insomnia
Sleep-onset insomnia stops someone from falling asleep when they initially go to bed for the night, so they spend a long time awake before finally going to sleep. This can happen either short- or long-term.
Sleep-maintenance insomnia
Failing to stay asleep through the night is called sleep-maintenance insomnia. This type is more common in middle-aged and older adults, and can also be acute or chronic.
Mixed insomnia
Some people have issues with both falling asleep and staying asleep all night.
Paradoxical insomnia
Those with paradoxical insomnia may feel like they barely slept at all, while in reality, they actually got more sleep than they think.
Summary
| Type of Insomnia | Description |
| Chronic insomnia | 3+ times/week, and for 3+ months, sleeping difficulties cause waking symptoms like fatigue and attention issues. |
| Acute insomnia | Sleep difficulties occur less than 3 times/week or for less than 3 months. |
| Sleep-onset insomnia | Trouble falling asleep |
| Sleep-maintenance insomnia | Waking up too early or having trouble staying asleep through the night |
| Mixed insomnia | Struggling to fall asleep and stay asleep |
| Paradoxical insomnia | Underestimating the real amount of sleep |
Common Causes of Insomnia
For some people, there is no clear underlying cause of their insomnia. But in many cases, insomnia is linked to a health problem/medical condition, schedule, environment, lifestyle, stressor, or emotional trigger. Let’s detail some common causes of insomnia:
- Psychological causes
- Depression
- Anxiety
- PTSD
- Schizophrenia
- Bipolar disorder
- Life events
- Job loss or change
- Divorce
- Moving
- A traumatic event such as the death of a loved one
- Pregnancy, PMS, or menopause
- Pain or discomfort
- Conditions
- GERD
- COPD
- Sleep apnea
- Restless leg syndrome
- Chronic pain
- Hyperthyroidism and other endocrine problems
- Alzheimer’s and other forms of dementia
- ADHD and ASD
- Medications
- Allergy, asthma, cold medicines
- Antidepressants
- High blood pressure medication
- Other substances
- Caffeine
- Alcohol
- Tobacco
- Illicit drugs
- Genetic factors
- Sleep schedule changes
- Jet lag
- New shift at work
- Poor sleep habits or environment
Psychological causes
Think about your current mental and emotional health. Are you going through a significant or distressing period in your life? Do you suffer from any psychological conditions?
Psychological influences can lead to insomnia. This includes conditions like anxiety, depression, PTSD, schizophrenia, and bipolar disorder. Additionally, we can have psychological reactions to traumatic experiences and life stressors such as job loss/change, health diagnoses, the deaths of someone close, moving, and divorce.
Physical causes
If you take certain medications or live with certain medical conditions, these can be physical contributors to insomnia. Antidepressants and meds that treat hypertension, allergy, asthma, and colds can also bring on insomnia, people with GERD, COPD, sleep apnea, restless leg syndrome, chronic pain, hyperthyroidism, and endocrine problems, ADHD, ASD, Alzheimer’s, Parkinson’s, and other forms of dementia can also have insomnia.
Additionally, natural hormone changes that occur during pregnancy, PMS, and menopause are potential physical causes of insomnia.
Lifestyle/Environmental Causes
Sometimes our environment, lifestyle choices, revised schedule, and bedtime habits can interrupt our regular circadian rhythm which tells our brains and bodies when it’s time to sleep:
Schedule
The mind and body are programmed Based on learned routines as well as the natural release of hormones. When we experience unconventional schedules such as night shifts or rotating shifts, it makes it difficult for us to get adequate sleep. This is especially true when we travel to different time zones and feel jet lag.
Lifestyle
Using or overusing caffeine, alcohol, tobacco, and illicit drugs can easily disrupt sleep patterns and lead to insomnia.
Environment
Our nighttime routines and environment play a major role in maintaining quality sleep and an optimal sleep schedule.
For obvious reasons, it can be harder to sleep in a setting with disturbing noises, too much light, or uncomfortable temperatures. Additionally, when pets join us in bed, they can also disrupt sleep.
Sleep Hygiene
Someone with poor sleep hygiene may have a sporadic bedtime routine, drink too much caffeine during the day or too late in the day, exercise too close to bedtime, spend too much screen time before bed, or not give themselves enough time to relax and clear their mind before sleeping.
What are the Risk Factors for Insomnia?
Because certain lifestyles, habits, life events, medications, medical conditions, and psychological factors can cause insomnia, certain people have a higher risk of experiencing insomnia.
So if any of the following variables apply to you, you might be more likely to have insomnia:
Age, Gender, and Socioeconomic Status
Those with lower socioeconomic status are at pronounced risk for insomnia. Older individuals over 60 are more prone to insomnia, possibly because they are more likely to suffer from underlying health issues. Women are also more likely to have insomnia, particularly during hormonal changes from PMS, menopause, and pregnancy.
Lifestyle
A sedentary lifestyle, night shifts, rotating shifts, and long-distance travel (particularly with time changes) are some of the other risk factors for insomnia. Screen time around bedtime and the use of caffeine, alcohol, and drugs are also associated with increased insomnia risk.
Medical Conditions
Psychological conditions including anxiety and depression often interfere with sleep, increasing the risk of insomnia. Additionally, insomnia is more common in those with developmental disorders and long-term illnesses.
Medications
Here are some of the medications with links to heightened insomnia risk:
- ACE inhibitors
- Alpha-blockers
- ARBs
- Beta-blockers
- Cholinesterase inhibitors
- Corticosteroids
- Glucosamine and chondroitin
- Non-Sedating H1 agonists
- SSRI antidepressants
- StatinsInsomnia Symptoms: What is it Like to Have Insomnia?
Sleeping helps our bodies and minds reset and recover to prepare us for the day ahead. So when you’re unable to sleep, especially often and/or over long periods of time, it takes a serious toll on mental and physical functioning.
Whether it’s an issue with sleep-onset or sleep maintenance, chronic or acute, insomnia symptoms can look like this:
Sleepiness during the day
Daytime fatigue can set in fast as someone gets further and further behind on sleep. This lethargy can lead to difficult mornings, overdependence on caffeine, and lower motivation at work or school.
Problems with concentration or memory
Seven to nine hours per night is the optimum sleep duration for mental function. Insufficient or disrupted sleep can stall the natural sleep cycles the brain depends on to process learning, emotions, and memory to remain productive day-to-day.
This is why sleep deprivation from insomnia often leads to cognitive decline, particularly with focus and memory.
Irritability
Insomnia’s effects on the brain directly impact the sufferer’s mood. Plus, exhaustion and impaired cognition can compound the negative mood as the person struggles to get through daily tasks.
Insomnia Diagnosis
If you’re having a hard time sleeping to the degree it’s harming your energy levels, mental performance, mood, work, or relationships, get medical attention.
When you see a doctor for trouble sleeping or talk to a sleep doctor via telemedicine, here’s what you can expect regarding the next steps:
Assessment and/or physical examination
Before you go to the doctor, it’s a good idea to prepare a few questions to ask during your appointment:
- Could my medications be causing insomnia?
- What can I do to improve my sleep?
- What other sleep disorders might I have?
- What would my bed partner say about my sleep?
The doctor will inquire about your medical history and any prescribed or over-the-counter medications, or supplements, in case it helps them identify any risk factors or potential underlying causes. They’ll likely ask about your sleep habits, and conduct a sleep questionnaire to assess your insomnia symptoms and their severity.
Sleep diary
During your initial insomnia assessment, the doctor might ask you to keep a sleep diary to rule out other sleep disorders and/or help identify the source of your sleep disturbance.
Your sleep diary might help you track your bedtime, wake time, naps, and caffeine use to gain insights into your sleep problems. The doctor could also suggest using a wearable device such as a sleep-tracking ring and/or app to help track sleep-wake patterns.
The Restore Sleep app which is used in conjunction with the Restore Ring provides a place for the wearer to record notes about their sleep each night.
Sleep studies
Sleep studies are not required to diagnose insomnia. But if your doctor suspects an underlying sleep disorder like sleep apnea, they may recommend a sleep study.
A sleep study, or polysomnogram, is when you sleep overnight at a facility (sleep lab) to monitor brain waves and other markers as you sleep. Alternatively, many patients will undergo at-home sleep testing for its convenience and lower cost.
Insomnia Treatment
We ask that you resist the temptation to skip the diagnosis step and instead, self-medicate. Insomnia can accompany dangerous underlying conditions and complications, so medical attention is vital for sleep problems that are interfering with your life. Besides, over-the-counter sleep aids can come with side effects and dependency and eventually stop being effective
To be most effective, we ask that you follow the treatment regimen your doctor has discussed with you:
Lifestyle Modification
Especially for short-term symptoms, your insomnia may ease by simply adjusting your lifestyle to improve sleep. This could include cutting down on alcohol, tobacco, and caffeine, being more physically active, or practicing better sleep hygiene.
Sleep hygiene means consistent bedtimes and wake times, a relaxing, screen-free evening routine, and optimizing your sleep environment by making it dark, quiet, and comfortable. To learn more about sleep hygiene, click: here:
Medications
Short-term, your doctor may prescribe medication to help you get better sleep and function better every day. However, they probably won’t want you to use medication alone for an extended time, as the medication isn’t the first choice to treat chronic insomnia.
That’s partially because insomnia medications can have a lot of side effects such as drowsiness, balance and motor coordination difficulties, and problems with memory and focus. 80% of people taking prescription sleep aids get at least one of these side effects the day after.
Melatonin
There is evidence that supplemental melatonin can help some people sleep better without serious adverse effects. Melatonin is a hormone that is released naturally in the evening and makes us feel drowsy. It influences our Circadian Rhythm, the internal clock responsible for sleep patterns, helping people fall asleep faster, stay asleep, and fall back asleep after waking up at night.
Melatonin is available without a prescription, and it’s not FDA regulated. As a result, some melatonin supplements have been found to have labels with inaccurate dosage information and ingredients (like dangerous undisclosed serotonin).
So talk to your doctor before trying melatonin for insomnia, so they can guide you to trusted sources and the optimal dosage for you.
Cognitive-Behavioral Therapy
Especially for chronic insomnia, cognitive behavioral therapy, or CBT-I, is the gold-standard insomnia therapy.
CBT for insomnia assists patients with underlying psychological factors, encouraging them to control worrying and negative thoughts that keep them awake. This approach also teaches practical sleep habits.
- Stimulus control- Consistent bedtime, avoiding naps, reserving the bedroom for sleep, and leaving the bedroom if you can’t fall asleep in 20 minutes
- Sleep restriction- Refraining from lying awake in bed, which might initially increase sleep deprivation so you’re more tired the following night
- Sleep hygiene- Regular exercise, calming nightly routine, reduced caffeine, tobacco, and alcohol
- Sleep environment- Quiet, dark, cool bedroom with no TV or clocks
- Relaxation training- Calming down through meditation and muscle relaxation
- Passively awake- Letting go of the conscious intention to sleep to ease worry and relax
- Biofeedback- Observing and adjusting biological cues like heart rate and muscle tension, sometimes using a wearable device
Addressing Underlying Causes
If the root of your insomnia is a physical contributor such as a medical condition, medication, or changes in hormone levels, your doctor may help you manage the underlying physical cause.
Insomnia Complications
Seeking treatment is so crucial because untreated insomnia can pose a detrimental risk to your overall health in the long run. The potential health complications include:
- Worsening insomnia– A cycle of sleep deprivation and escalating sleep anxiety can turn short-term insomnia into a chronic problem
- Depression and other mood disorders– The brain isn’t getting its needs met, leading to low mood, while other insomnia symptoms are likely to compromise one’s personal and work life
- Accidents and injury– Drowsiness and deficits in alertness, reaction time, and physical coordination can increase slips, trips falls, and car accidents Without adequate sleep, the brain and body work harder to self-regulate, causing a host of medical issues:
- High blood pressure, heart disease, cardiovascular disease, and stroke
- Diabetes
- Weight gain and obesity
11 Tips to Prevent Insomnia
How can we prevent insomnia from developing out of mild sleep disturbances or from returning once we’ve got it under control? Take these steps to keep insomnia at bay:
- Maintain regular sleep and wake times, avoiding naps
- Eliminate all screen use in bed including an hour prior to bedtime
- Minimize alcohol, nicotine, and caffeine, especially later in the day
- Don’t eat big meals within 2-3 hours before bedtime
- Exercise, but don’t work out unless it’s more than 3-4 hours before bedtime
- Keep the bedroom quiet, dark, and comfortable; consider using a sleep mask, earplugs, a fan, or white noise to help
- Establish a relaxing nightly ritual such as stretching, medication, or reading a book.
- Don’t do any work or entertainment in bed; reserve it for sleeping so your mind doesn’t associate bedtime with alertness
- If you’re not tired when it’s time to go to sleep, get out of bed, and do something that relaxes you like reading
- If you cannot let your mind rest, try this. As you’re getting ready for bed, write down every idea, to-do list, and worry you may have. By pouring your thoughts onto paper, you’re giving your brain a chance to let go of them for the night. Once you have them written down, you can rest easy, knowing that you can pick back up with your ideas in the morning. Track your sleep habits and patterns using a diary, app, and/or wearable device to identify the problem if your sleep starts declining

FAQs About Insomnia
How do you know if you have insomnia?
You may have insomnia if your inability to sleep recurs three or more nights per week and/or lasts longer than three months, and is negatively affecting your life.
How many hours of sleep is insomnia?
Most adults need between 7-9 hours of sleep each night in order to feel alert and well-rested. Those with insomnia usually get significantly less than that. The hours of sleep you get play a role in insomnia severity, but hours of sleep do not diagnose or rule out insomnia.
How do I stop my insomnia?
To stop insomnia, consider making the appropriate lifestyle and sleep hygiene changes, and talk to your doctor about diagnosing and treating your insomnia.
Basic changes can help minimize insomnia by reducing caffeine, alcohol, and tobacco, making the sleep environment as comfortable and calm as possible, exercising regularly, but not too close to bedtime, and taking time at the end of the day to slow down without screens or distractions.
What can I drink to sleep faster?
Avoid alcohol and caffeinated beverages, as these disrupt sleep. Some people fall asleep faster after drinking soothing caffeine-free teas with chamomile, peppermint, and valerian. Cherry juice, turmeric beverages, and almond milk can also help people fall asleep naturally.
Can insomnia go away on its own?
For some people, insomnia may dissipate on its own, especially if it’s just short-term insomnia. Speak with the doctor if insomnia lasts longer than three months.
Can insomnia be cured?
Yes, many people recover from insomnia with cognitive-behavioral therapy and modifying their bedtime routines. Is insomnia a mental disorder?
Insomnia is considered a sleep-wake disorder. Some cases of insomnia are diagnosed using the criteria of the DSM-5, which categorizes mental disorders., At what age does insomnia start?
Insomnia can affect people at any age, from children to older adults. In children, sleep disturbances most often begin at the age of 11 or 12 as this is when your child starts to release melatonin later at night than when they were younger.
What’s getting between you and restful sleep?
With insomnia, half the battle tends to be finding the source of the problem. Whether your sleep challenges originate from bad habits, a condition or medication, a tough stage of life, or psychological distress, help is available.
Take steps to seek medical attention and treat your insomnia so your sleep and quality of life can make a comeback. With the prevalence of telehealth solutions and digital health apps these days, getting help with insomnia has never been easier or more convenient.
You can contact a healthcare professional or specialist and start fixing the problem without even leaving the house.