Sleep Apnea: Types, Causes, Symptoms, Treatment
You’re tired of being tired all the time. It doesn’t matter how early you go to sleep or how regular your nighttime routine is, you always wake up unrested. It likely affects your partner’s sleep too when you keep them up all night with your snoring and sudden waking.
As much as it compromises your well-being, sheer exhaustion isn’t the only danger of living with the sleep disorder called sleep apnea. Along with symptoms like headaches, dry mouth, and chest pains, sleep apnea is linked to cardiovascular disease, pulmonary hypertension, liver problems, and many more chronic healthcare issues.
So if you know or suspect you have sleep apnea, it’s vital to seek medical attention. Educate yourself on the signs and symptoms, causes, risk factors, diagnosis, and treatment options,
Everything you need to know about sleep apnea is right here in this guide. Keep reading to learn more about the condition and you will be one step closer to managing sleep apnea for a better quality of life.

What is Sleep Apnea?
Sleep apnea is a sleep disorder causing the airway to collapse and the sufferer to stop breathing occasionally while they sleep. Then, your brain wakes you up, prompting you to resume normal breathing.
If this happens to you, you probably won’t remember this is happening, so many people don’t even know the problem exists unless a bed partner alerts them to it.
How Does it Harm Physical and Mental Functioning?
Though the survival reflex to wake up re-starts your breathing, it interferes with the natural sleep cycle, so you can’t get restful sleep. Every night, you’re missing out on the healthy sleep you need.
To understand how sleep apnea is so detrimental to people’s sleep, let’s review the human sleep cycle:
- Stage 1 ‘light sleep’ starts right after you first fall asleep, accounting for 5% of your sleep time.
- Stage 2 is a deeper stage of sleep comprising 45-50% of sleeping time, depending on age.
- Stage 3 is called ‘slow wave sleep,’ and it takes up 35% of the time you’re asleep. This is the deepest stage when it’s hard to wake up, and you’ll experience mental fog if you do wake up.
- REM (rapid eye movement) sleep is when you dream.
When you fall asleep, you start in Stage 1, then move back and forth between Stages 2 and 3 before entering REM. Then after a while in REM, the process repeats four to five times per night (over about eight hours). Each cycle takes 90 to 110 minutes.
During the sleep cycle, your brain is always monitoring your body and working to adjust heart rate, blood pressure, and breathing. If you stop breathing due to sleep apnea, it can happen at any stage. Your blood oxygen levels drop, triggering your brain’s response to take a breath in order to replenish the oxygen in your blood.
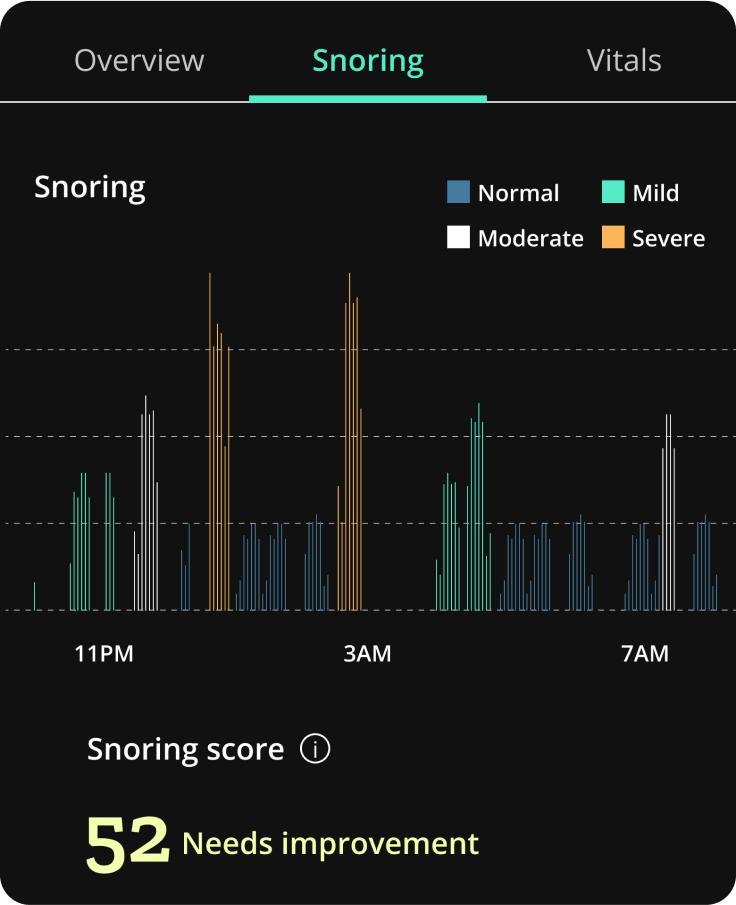
Mild sleep apnea wakes a person up 5-15 times per hour on average, and depending on symptoms, may or may not require treatment. With moderate sleep apnea, people tend to have 15-29 events per hour. People with severe sleep apnea wake up 30+ times every hour, adding up to at least 240 times during eight hours of sleep.
The brain tries to resume the sleep cycle, but depending on sleep apnea severity, it can profoundly compromise the sleep cycle impacting physical and mental functioning.
This is because the deep sleep stages are when you process memories, learning, and emotions. You need to spend enough time in these stages for your body to recover, regulating blood sugar and metabolism, energizing the immune system, and detoxifying the brain.
Types of Sleep Apnea
There are two main types of sleep apnea. Obstructive and central sleep apnea have different causes, prevalence, risk factors, and treatments:
Obstructive Sleep Apnea (OSA)
Affecting an estimated 10% to 30% of adults in the U.S., obstructive sleep apnea is the most common type. People with obstructive sleep apnea have slackened airway muscles and tissues that constrict or cause the airway to collapse so that air cannot freely move to the lungs during sleep.
This airway obstruction prompts the person to wake up, engage the throat muscles, and gasp for air, often with snorting or choking sounds. They may not even remember this occurring even though it may happen hundred of times each night.
Central Sleep Apnea (CSA)
Central sleep apnea is less common, found in less than 1% of people. In CSA, a communication failure between the brain and muscles involved in respiration causes episodes of paused, slowed, or shallow breathing during sleep. CSA is more common in those with heart failure, or who have certain neurological disorders.
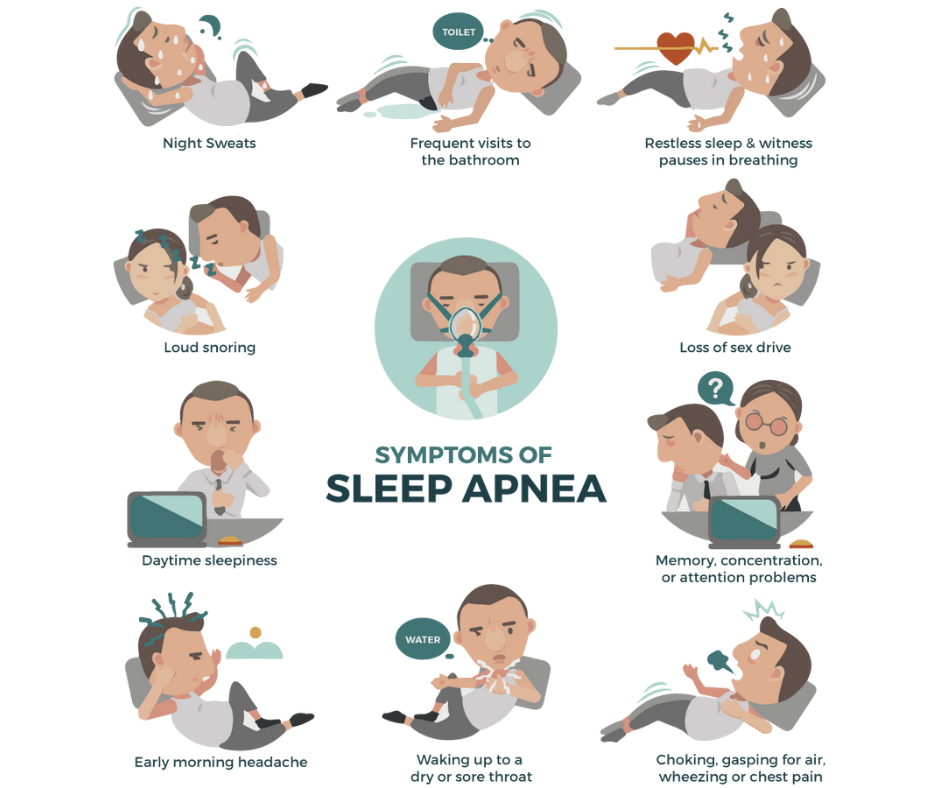
Signs and Symptoms of Sleep Apnea
So, how do you know whether you might have sleep apnea and should seek treatment? Firstly, be aware that sleep apnea can present differently depending on the type (OSA vs. CSA) and the individual case.
Also, many cases of sleep apnea go undiagnosed because the individual doesn’t realize they’re having symptoms. You may want to ask your partner if you display any sleep apnea symptoms while sleeping. For those who don’t share a bed, wearing an oximeter at night can alert you to possible sleep-breathing issues.
Here are some of the signs and symptoms sleep apnea sufferers and their families might notice:
Obstructive Sleep Apnea Symptoms
- Excessive daytime sleepiness
- Loud snoring, gasping, or choking at night
- Headaches lasting several hours in the morning
- Dry mouth
- Restless sleep
- Frequent urination throughout the night
- Impaired focus, memory, and cognition
Central Sleep Apnea Symptoms
- Abnormal breathing patterns with slowing, accelerating, and pausing
- Restless sleep or waking at night
- Sudden shortness of breath or chest pains during sleep
- Morning headaches
- Excessive fatigue during the day
- Impaired focus
Causes of Sleep Apnea
Let’s go into a little more detail about the causes of obstructive and central sleep apnea:
Obstructive Sleep Apnea
When the muscles in the back of the throat relax during sleep, upper airway obstruction occurs due to:
- Negative collapsing pressure while inhaling
- Narrowing the area behind the palate (roof of the mouth) while exhaling
Both of the above causes of airway obstruction in OSA are often related to increased body mass index (BMI). As anatomy differs in each person, we also see OSA occurring in those who are slender, have recessed jaws, small mouths, and/or and large tongues.
Central Sleep Apnea
Central sleep apnea is a sleep disorder defined by an increased number of reductions or pauses in breathing during sleep due to a lack of effort from the muscles that control breathing. These interruptions in normal breathing can occur sporadically throughout the night or in a cyclical pattern and show a decline in oxygen levels as the patient makes no effort to breathe.
[ Trusted Source Medscape is an online destination for healthcare professionals worldwide, offering expert perspectives, drug and disease information, and professional education. View Source ]
Although CSA involves pauses in breathing during sleep, not all such pauses indicate CSA. People who do not have the disorder naturally experience some pauses in breathing. These harmless interruptions occur while transitioning from sleep to wakefulness or after a deep sigh and do not meet the criteria of a sleep-related breathing disorder.
What are the Risk Factors for Sleep Apnea
Certain individuals are at an elevated risk for sleep apnea. Know what the risk factors are so you can assess how likely you are to have either OSA or CSA.
Obstructive Sleep Apnea Risk Factors
If any of the following apply to you, you may be more prone to obstructive sleep apnea:
- Obesity/BMI and neck circumference: Those with excess weight and/or thicker neck circumference can have narrower airways or fat deposits around the upper airway obstructing breathing. 20% of obese people have sleep apnea compared to just 3% of people with a normal weight.
- Narrowed airway: Some people, especially children can have enlarged tonsils or adenoids blocking the airway.
- Sleeping position: In some cases, sleeping on one’s back can make soft tissues press down onto the windpipe.
- Being male: Men are two to three times more likely than women to have sleep apnea. Roughly 25-30% of men in the U.S. meet the criteria for obstructive sleep apnea and only 9-17% of women. After menopause, women are on par with men for developing sleep apnea.
- Alcohol, sedatives, and tranquilizers: Certain drugs can worsen obstructive sleep apnea by relaxing the throat muscles.
- Smoking: Smokers are three times more likely to experience obstructive sleep apnea due to upper airway inflammation and fluid retention.
- Nasal congestion: Those who have trouble breathing through their nose are more likely to develop sleep apnea due to anatomy or allergies.
- Hypothyroidism is associated with obstructive sleep apnea as it may contribute to upper airway obstruction.
- Acromegaly is a hormonal disorder of the pituitary gland leading to enlarged body parts, and there appears to be a relationship between acromegaly and OSA.
- Other medical conditions associated with increased OSA risk include congestive heart failure, high blood pressure, type 2 diabetes, PCOS, prior stroke, asthma, and other lung diseases.
Central Sleep Apnea Risk Factors
There is some overlap in the risk factors for central sleep apnea:
- Age: Middle-aged and older individuals (65+) have a higher risk of central sleep apnea.
- Sex: Males are also at higher risk for central sleep apnea.
- Narcotic pain medicine: Taking opioids like methadone increases CSA risk.
- Altitude: Since oxygen is less available at high altitudes, altitude is associated with increased central sleep apnea risk.
- Medical conditions: Other risk factors include heart disorders like congestive heart failure, prior strokes, excess growth hormone, neurological conditions, kidney failure, and infections and injuries of the brain stem.
Sleep Apnea Diagnosis
If you believe you might have OSA or CSA, you should go to the doctor and tell them about your concerns. You may be referred to a sleep specialist to be evaluated and then diagnosed so that a specific treatment can be prescribed that would improve sleep quality.
Health History
In an initial evaluation, the doctor may ask you and your partner about any sleep apnea symptoms. They’ll take your health history and have you complete sleep questionnaires to understand your issues and concerns and will check for sleep apnea risk factors Physical Assessment
A physical exam helps your Health Care Provider assess your general health for potential underlying conditions or factors that could contribute to sleep apnea like neck circumference, and may also examine your nose and throat.
Sleep Study
The most common and reliable sleep apnea test is an overnight sleep study or polysomnogram at a medical facility, also known as a sleep lab or sleep clinic.
As you sleep at the facility for the night sensors monitor your heart rate, blood oxygen levels, breathing, brain waves, sleep stages, and muscle movement.
This helps the doctor or sleep specialist identify the type and frequency of breathing disruptions, make an OSA or CSA diagnosis, and determine the severity.
At-Home Testing
Not everyone is eligible for an in-lab sleep study. As an alternative or as a preliminary measure preceding an in-clinic polysomnography follow-up, you may undergo at-home testing.
At-home sleep testing also measures sleep breathing issues, but it doesn’t capture EEG, thereby providing less data. Most patients prefer it for its convenience, comfort, and less out-of-pocket cost. T results are interpreted by a sleep doctor and then recommendations are made for therapy if needed.

How is Sleep Apnea Treated?
The results of your testing, diagnosis, sleep apnea type, and severity will determine the best treatment approach. Most are covered by insurance, and some are not.
Treatment for Obstructive Sleep Apnea
- Positive airway pressure (PAP) therapy: Almost all obstructive sleep apnea patients are prescribed positive airway pressure therapy, particularly for those with moderate to severe OSA. This treatment keeps the airway open using pressurized air that pumps from a machine through a hose into a mask that is worn over the nose or mouth or both. The sleep study may include a process called titration to precisely calibrate the air pressure that is most beneficial to the patient.
- A CPAP (continuous positive airway pressure) device sends an airstream with a consistent pressure level.
- Variable air pressure devices:
- BiPAP (bi-level positive airway pressure) device- This PAP device provides a higher inspiratory pressure and a lower expiratory pressure making it easier for patients to breathe with the air pressure.
- APAP (auto-titrating positive airway pressure) device- many patients receive this type of PAP device because it provides for a range of pressures that best fit the patient’s needs. This device also reduces the need for patients to go to the sleep lab for a titration study.
- Oral Appliances: These are mouthpieces designed to hold the jaw or tongue in the forward position to open the airway and treat less severe OSA. Customized oral appliances are provided by specialized dentists and can reduce snoring and improve breathing but may not be as effective as PAP therapy. However, this is an option for people primarily with mild or moderate OSA or those who don’t respond or struggle to use PAP devices. NOTE: There are new, alternative therapies and innovations now available that many patients prefer. Restore Sleep has access to these new treatments and will make these available to patients.
- Surgery: Patients with tissue obstructing the airway might have surgery to expand the airway by removing some tissues in the throat. Another type of surgery implants a device to stimulate a nerve that controls the tongue, moving it out of the airway during sleepThis option is for moderate to severe OSA patients who cannot tolerate PAP devices.
- Lifestyle changes: The following lifestyle changes can manage or eliminate sleep apnea symptoms:
- Weight loss/reducing BMI: A 10% decrease in body weight can substantially improve sleep apnea symptoms in those who are overweight or obese.
- Exercise: Even without losing weight, exercising regularly can decrease OSA symptoms.
- Positional sleep Aids- Change sleeping position. For example, Back sleepers with OSA should try to get used to sleeping on their side to keep soft tissues in the throat from obstructing the airway.
- Smoking and alcohol: Reducing or eliminating cigarettes and/or alcohol can improve obstructive sleep apnea.
Treatment for Central Sleep Apnea
Central sleep apnea can occur with an underlying medical issue. So for mild disruptions from CSA, simply treating the underlying cause may be enough.
PAP devices are also prescribed to people with central sleep apnea to steady breathing during sleep. Medications may be used to speed up the patient’s breathing. Or, the doctor may prescribe supplemental oxygen therapy.
Additionally, CSA can be treated with ASV (adaptive servo-ventilation), similar to CPAP therapy. ASV continuously monitors sleep breathing and uses intricate algorithms to respond to breathing patterns with airway pressure in real-time.
For CSA patients who are unable to tolerate this therapy, the remedē implant stimulates the phrenic nerve that controls breathing and works throughout the night to keep the patient breathing on their own in spite of the CSA.

Sleep Apnea Complications
It might sound daunting to go through all the testing, diagnostics, and treatment. But it’s worth it to reduce the serious risks associated with sleep apnea.
It’s not just a matter of toughing it out in the face of exhaustion. Untreated, sleep apnea can have life-threatening complications that further endanger your health and well-being:
- Impaired concentration and memory
- Mood swings, especially irritability, and depression
- Drowsy driving causes car accidents
- Metabolic disorders like type 2 diabetes
- Pulmonary hypertension- high blood pressure in the lungs’ arteries causes strain on the heart
- Cardiovascular disease- high blood pressure, stroke, heart failure, heart disease, sudden cardiac death
- Arrhythmia/atrial fibrillation- disrupts blood flow through the upper left heart chamber, causing pooling blood, blood clots, and possibly stroke
- Nonalcoholic fatty liver disease- increased fat deposits in the liver causing serious damage
- Anesthesia, surgery, and medication complications
Summary
Here’s a quick guide summarizing OSA and CSA:
| Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) | |
| Cause | Airway obstruction during sleep | Faulty signaling between the brain and the muscles that control breathing |
| Symptoms | Loud snoring, choking, gasping at night, restless sleep, daytime sleepiness, morning headache | Irregular breathing, pauses in breathing during sleep, difficulty staying asleep, morning headache |
| Risk Factors | Sex, excess weight/obesity, large neck circumference, smoking, alcohol | Sex, age, heart failure, stroke, high blood pressure, medications, altitude |
| Diagnosis | A sleep study (polysomnography) | A sleep study (polysomnography) |
| Treatment | PAP therapy, lifestyle change, oral appliances, surgery | PAP therapy, medication, oxygen, ASV |
FAQs About Sleep Apnea
How serious is severe sleep apnea?
Severe sleep apnea can disrupt an individual’s breathing and sleep more than 30 times every hour, which adds up to over 240 times in eight hours. This can cause severe symptoms like fatigue, cognitive decline, and very dangerous health complications.
Can long-term untreated sleep apnea decrease IQ/intelligence?
Sleep apnea can cause cognitive decline, impacting focus and memory, but does not appear to affect IQ.
Can you live with untreated sleep apnea?
Many cases go undiagnosed and untreated because the sufferers have symptoms but don’t realize they’re stemming from sleep apnea. But leaving sleep apnea untreated can be detrimental to health and well-being, leading to serious, life-threatening consequences.
How common is sleep apnea without snoring?
In CSA, snoring isn’t one of the most common symptoms. However, OSA is usually accompanied by snoring. If you don’t snore, there’s not enough information to rule out sleep apnea.
Is there a personal Sleep Apnea monitor/test you can buy?
Personal sleep apnea tests are portable monitors for breathing and oxygen levels to detect pauses in breathing. At-home sleep apnea tests can be one piece of a formal medical diagnosis and treatment monitoring.
Are you ready to live free from sleep apnea symptoms?
Don’t put it off any longer. If you’re wondering whether you have OSA or CSA, it’s important to talk to your doctor. There’s no need to suffer through constant fatigue, mood disturbances, cognitive difficulties, or mounting health problems.
The most common sleep apnea treatments provide prompt results, symptom relief, and reduced risk of complications. So the sooner you seek out diagnosis and treatment, the sooner you can enjoy a better quality of life.

